 For a surgeon who has successfully treated prostate cancer in many thousands of men by removing their prostate gland, the idea that science might one day be able to regenerate this gland using stem cells is a foreign one — and yet highly intriguing. But this advancement is just one of many potential treatments for prostate cancer or benign prostate enlargement that may eventually arise from important new research on the cellular building blocks of prostate gland development.
For a surgeon who has successfully treated prostate cancer in many thousands of men by removing their prostate gland, the idea that science might one day be able to regenerate this gland using stem cells is a foreign one — and yet highly intriguing. But this advancement is just one of many potential treatments for prostate cancer or benign prostate enlargement that may eventually arise from important new research on the cellular building blocks of prostate gland development.
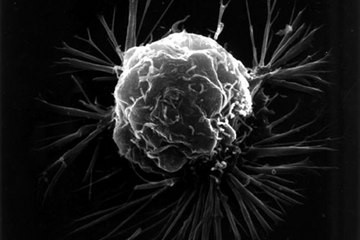
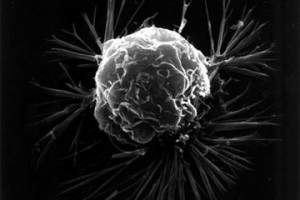
In a study published Feb. 11 in the journal Stem Cell Reports, scientists from the University of York in England detailed their discovery of a “signaling pathway,” a set of signals that tell proteins inside stem cells how to evolve into prostate tissue cells called basal cells and luminal cells. The researchers learned there are 80 genes involved in this process, and that the main signals responsible for activating prostate development are retinoic acid and male sex hormones — the balance of which are disrupted in prostate cancer.
Until now, all the information clinicians have had about the prostate gland has been on a macroscopic level, dealing with the prostate gland itself and the location of cancerous tumors or other anatomical features. But this breakthrough sheds light on the prostate gland on a microscopic level, unearthing cellular and genetic information that will almost certainly change the future of prostate cancer treatment.
Understanding the 80 genes and signaling mechanism needed for prostate gland growth is a key in the lock for researchers genetically mapping prostate tumors. Instead of treating cancer by using radiation to kill malignant cells or by surgically removing the gland — which has proven highly effective — clinicians may be able to interfere with tumor genes themselves, thereby cutting off cancer growth.
Current hormone treatments reduce men’s testosterone levels to slow down the disease, but at a huge personal cost, causing dramatic side effects such as hot flashes, erectile dysfunction, fatigue and loss of muscle mass. These effects might all be avoided if we can throw cancer cell proliferation out of sync using gene therapies. And of course, another exciting possibility is the potential to someday replace cancerous prostate glands with healthy versions grown from stem cells, something already being attempted for other organs such as the heart, bladder and liver.
Prostate cancer treatments are of course the natural focus, but these research revelations might also affect the millions of men around the world coping with benign prostate enlargement, a highly common consequence of aging that causes troublesome symptoms such as urinary urgency, slow urinary stream and increased urination, particularly at night. If this new knowledge about prostate development could be used to “freeze” prostate organ growth to rates seen in younger men, it would be a true anti-aging formula providing a higher quality of life for unprecedented numbers of people.
Implementing these new therapies could take years, and more research is undoubtedly needed to validate the scientists’ findings. But their discovery may indeed change the face of medicine. After I successfully performed robotic prostate removal surgery on anti-crime activist and Guardian Angels founder Curtis Sliwa in 2011, he joked to me, “If anyone wants to give me a prostate transplant, I’m listening.” If this new research paves the way to using stem cells to grow new prostate glands in coming years, maybe Sliwa’s wish can come true.
This article was originally published on Live Science.