Here are the 10 steps involved in having a skin biopsy.
When you notice a concerning rash or mole on your skin, the body’s largest organ, it’s a good idea to see a dermatologist to have it evaluated. Sometimes after checking the area, your dermatologist may recommend a skin biopsy.
Skin biopsies are an important part of verifying a diagnosis. For example, a biopsy is the only way for a doctor to confirm and determine the severity of a melanoma—the most serious type of skin cancer. A skin biopsy can also be used to confirm that a skin tumor is benign or to diagnose inflammatory skin conditions such as a drug-related rash or eczema.
Below, Yale Medicine dermatologist Jean Bolognia, MD, and dermatopathologist Jennifer McNiff, MD, explain what you need to know before having a skin biopsy. Here are the 10 steps involved:
1. A Dermatologist Checks Your Skin.
Patients see dermatologists for multiple reasons, including concern regarding a particular skin lesion or worsening of a rash. In addition, patients at risk for skin cancer have total body skin examinations performed at regular intervals. Sometimes a patient may be referred to a dermatologist by a primary care physician for more specialized expertise. If you have a skin concern, your dermatologist will evaluate it during an office visit, asking questions about your skin issue and how long you’ve had it.
2. The Dermatologist Decides If a Skin Biopsy Is Needed.
Biopsies of the skin are most commonly performed on an out-patient basis during an appointment with your dermatologist. After examining the rash or a lesion that the patient or the physician finds concerning, the patient is asked questions regarding its history. The dermatologist then determines if a skin biopsy is necessary. In the case of a rash, a fresh, but well-developed, lesion is chosen and if possible in a site of minimal cosmetic concern, if possible. Following a total body skin examination, the most worrisome lesion(s) are biopsied. Sometimes a biopsy may be done a week or two later if the skin condition is not considered severe or life threatening.
3. The Doctor Gives a Local Anesthesic.
The biopsy area is cleansed, usually with alcohol, and then a local anesthetic such as lidocaine is injected to numb the area, using a very fine needle. The lidocaine solution often contains epinephrine (to decrease bleeding) and sodium bicarbonate (to decrease the burning sensation). The patient will feel a slight pinch of the needle, and then a brief burning sensation as the anesthetic is injected. A feeling of pressure may also occur when the local anesthesia is injected into a relatively taut area of skin such as the fingers or toes. If the patient is apprehensive regarding the injection, a topical anesthetic can be applied for one to two hours prior to the procedure to reduce the associated pain.
4. The Dermatologist Performs the Correct Type of Biopsy.
The type of biopsy a patient needs is determined by the size and location of the lesion, the depth of the skin concern, and the information being sought based upon the most likely diagnoses. The dermatologist’s expertise is crucial in making this decision. Types of biopsies include:
- Shave biopsies are employed when the dermatologist suspects that the condition or tumor involves primarily the top layer of the skin (the epidermis). The biopsy specimen includes the epidermis and sometimes the superficial portion of the dermis (the second layer of skin). The scalpel blade is slightly angled when performing this procedure.
- Saucerization is performed if the dermatologist envisions that the disease or tumor extends into the upper or mid dermis. In this type of biopsy, the edge of the blade is at a greater angle relative to the surface of the skin. This type of biopsy is often done on the trunk.
- Punch biopsy is a technique that involves a circular blade that resembles a cookie cutter. It enters the skin with a gentle turning motion. A punch biopsy is performed when the disease or tumor is thought to involve the deeper dermis and/or when placement of sutures is planned.
- Excisional biopsy is performed when the disease or tumor is thought to involve the deeper dermis and perhaps the subcutaneous fat. In the case of a tumor, the goal is complete removal. Sutures are placed to close the wound. Sometimes the tumor is too large to remove in its entirety or a partial biopsy is adequate (for example, for inflammatory diseases) and an incisional biopsy is performed.
5. Post-Operative Care Is Given After a Skin Biopsy.
After your skin biopsy, you should take good care of the biopsied area at home. To speed healing, keep the biopsy site moist by applying an ointment which will prevent scabbing and minimize scarring. A small rim of redness is commonly seen at the edge of a healing wound but expanding redness, fever, chills, pus, or significant pain can be signs of an infection, which is uncommon.
How long healing takes varies and depends upon the size and depth of the biopsy, the anatomic site (the face heals much faster than the ankle), and any underlying medical conditions you may have. Most biopsy sites heal within 2 to 3 weeks.
6. The Biopsied Skin Tissue Is Sent to a Dermatopathology Laboratory.
Yale Medicine has an on-site dermatopathology laboratory where skin biopsies are evaluated. That means the laboratory specializes in skin pathology. At the lab, there are nine board-certified dermatopathologists who render the pathologic diagnoses. “I feel very strongly that my biopsies should be processed by laboratory technicians who have specialized training in handling delicate skin tissue,” says Dr. Bolognia, who is also a professor of dermatology for Yale School of Medicine. “In addition, I want the physicians who are providing the pathologic diagnoses to have subspecialized in dermatopathology.”
Yale Medicine’s dermatopathology lab deals only with skin tissue (no other types of tissue from other organs are analyzed), and it offers the largest academic group of board-certified dermatopathologists in the Northeast.
“Our specially trained technicians process the tissue with great care so that maximum information can be obtained when put on a microscopic slide and studied by a dermatopathologist,” says Dr. McNiff, who is the medical director of the Yale Medicine Dermatopathology Laboratory. Yale Medicine’s dermatopathology physicians have helped shape the practice of dermatopathology, by making new discoveries, publishing their work and really living in the field, Dr. McNiff says. This type of dedication, specialization and depth of resources has resulted in better diagnostic expertise and outcomes.
7. The Dermatopathology Lab Processes the Tissue.
The tiny, delicate pieces of skin are carefully embedded into paraffin wax. This creates a block that can then be cut, put on glass slides, stained, inspected, and photographed. “Our dermatopathology technicians know how to make this process as accurate and efficient as possible,” Dr. Bolognia says. For example, all pathology labs use special stains to determine specific types of cells, but Yale Medicine’s dermatopathology lab has more than 250 stains just for skin. If Dr. Bolognia biopsies a nevus (mole) with a darker portion that is clinically worrisome, the technicians will put special ink on the dark area. This ensures that the dermatopathologist will carefully assess the area of concern to the clinician. “The placement of ink on areas of concern within a nevus is not a common practice,” Dr. Bolognia says. “However, our dermatopathology laboratory offers this added service,” Dr. McNiff says. “We do special procedures that are intended to be helpful to the dermatologist.”
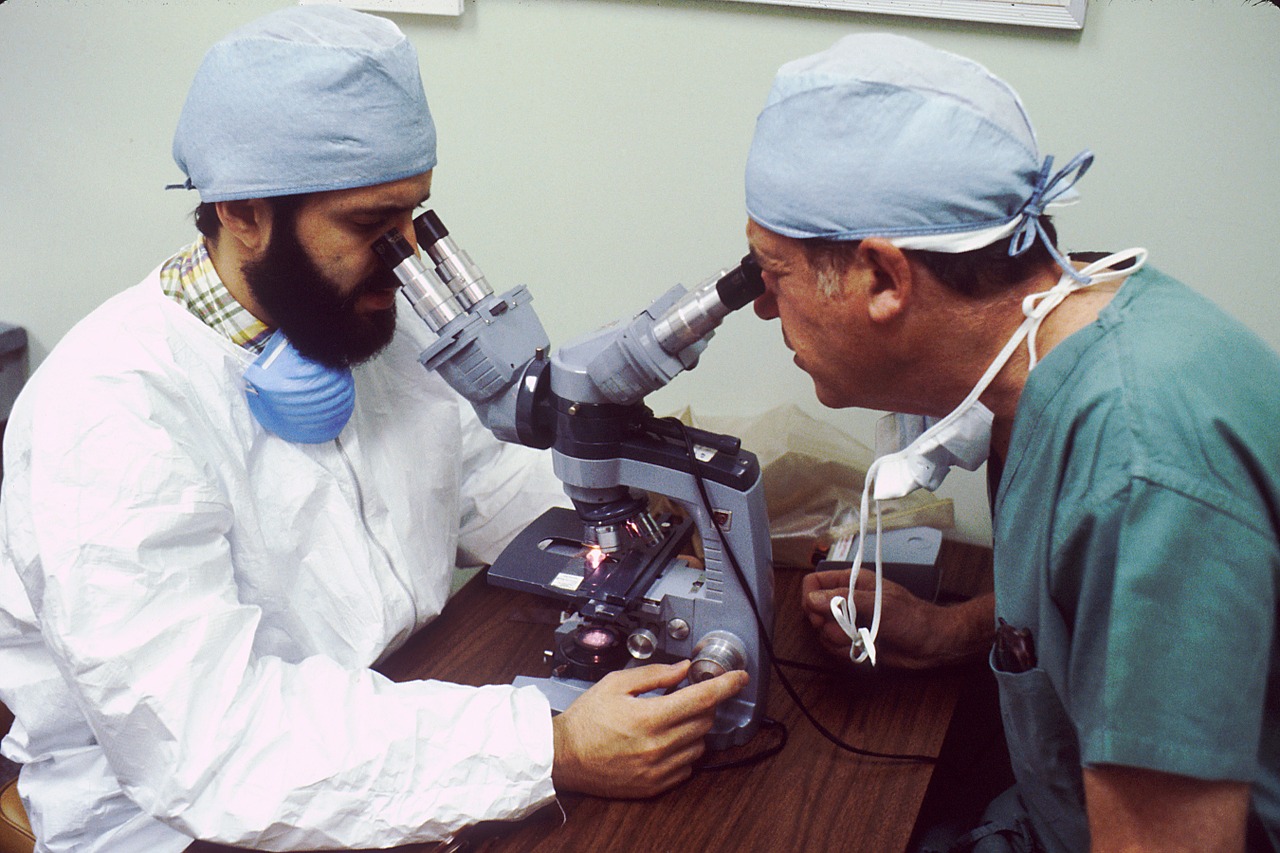
8. If the Case Turns out to Be a Puzzling One, It Is Discussed Among a Group of Dermatopathologists.
Yale Medicine’s dermatopathologists hold a daily consensus conference to discuss the most challenging cases. Their expertise is often sought by dermatologists, surgeons and medical oncologists throughout New England. “Every day, we all meet to go over a wide variety of challenging cases, seek multiple opinions, review relevant literature, and put our heads together to come up with an accurate diagnosis,” Dr. McNiff says.
9. The Dermatopathologist Creates a Report and Sends It to the Dermatologist.
If the dermatopathologist has questions about the patient, including specific medications or medical diseases, he or she calls the dermatologist who performed the biopsy before issuing the report. “What results is a conversation that’s helpful for both the dermatopathologist and the dermatologist,” Dr. McNiff says. This is not common in general pathology labs, and is not always routine in other specialized dermatopathology labs. Yale Medicine dermatopathologists are also given the opportunity to go with the dermatologist on rounds, which gives them insight into patient care.
10. The Dermatologist Contacts You with the Results of the Skin Biopsy.
If the results of the skin biopsy are benign, the dermatologist usually has results ready to share with the patient within a week. If the pathologic diagnosis is a benign tumor, then the patient is usually notified by mail or electronically via MyChart. In addition, those patients who sign up for MyChart have access to the actual pathology report as do their Yale Medicine physicans.
When results of a skin biopsy show a skin cancer or another condition that requires an explanation, then a call is placed to the patient. When the biopsy returns as a melanoma, the area must be re-excised with a goal of obtaining clear margins. Depending upon the depth of invasion of the melanoma, a discussion is also held regarding sentinel lymph node biopsy. The oncology section at Yale Medicine has an active melanoma unit and has expertise in a wide range of clinical presentations. “The patient will be treated appropriately with the most up-to-date therapies,” Dr. Bolognia says.
This article first appeared on the YaleMedicine blog.