Did you know that when you experience pain that is persistent, the central nervous system–that is your brain and spinal cord–plays an important role in how you feel?
According to the International Association for the Study of Pain, pain is ‘an unpleasant sensory and emotional experience’ in response to ‘actual or potential tissue damage.’ The pain you feel isn’t just experienced in the tissues; it’s actually created in the brain first. No brain, no pain.
Your brain interprets all kinds of messages that can lead to alarm bells ringing, two of which mechanisms are involved in pain. I’ll spare you the brain freeze of going through all of them, but let’s talk about those relevant here. One is called nociceptive, which is a message relayed by danger detectors called nociceptors in response to a painful stimulus coming from an organ and/or tissue. For example, if you stepped on a nail, you would know about it. (At least, I hope you would.) The second type of message is neuropathic, which is influenced by the central nervous system. Neuropathic pain is most commonly associated with persistent pain where your nervous system gets riled up and sensitive to even the slightest information it receives despite whether or not actual tissue injury is present.
Now, this explanation may seem pretty black and white but it gets more complicated when the many protective processes interplay to create a person’s experience of pain. These processes don’t occur in isolation. In fact, we now know there’s a lot of ‘crosstalk’ occurring at any given moment. Neuroscientists are only beginning to scratch the surface of these complex relationships.
What’s more it’s not all in your head. Your body parts have a ton of these detectors too. These sensors send electrical impulses up to your brain for interpretation, ultimately deciding whether or not you’re in need of protection. For example, when you’re talking it up with your buddies, what’s allowing you to hear what they’re saying? You might think your ear is how you hear and this is partially true. Your ear is a receptacle for sound to tunnel through, creating vibrations that stimulate little hair cells, exciting the nerves of your inner ear. This sends electrical signals to your brain, which interprets those vibrations into words that you can actually understand. Fascinating, right?! Well, the same goes for the sensations that you feel in the body.
Those little sensors are found everywhere: in your ligaments, joints, muscles, hair cells, bone, blood vessels, nerves, organs. The list goes on and on. These sensors respond to temperature, touch, pressure, stretch, movement, smell, sight, thoughts, stress, noise. Anything can be a trigger. They’re the same sensors that send messages to your brain signaling danger. Just like your brain interprets the sound that comes into your ear so that you can have a social interaction, it also interprets ‘danger’ messages so that it can protect you. Potential dangers can be anything that you perceive as a threat. They can be physical like a snake bite or they can be emotionally driven like the thought of being turned down for a first date.
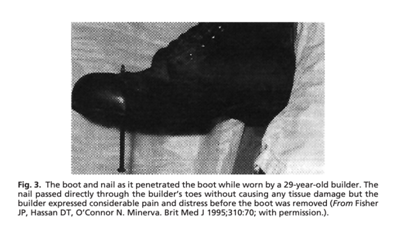
Pain is a conscious experience. Nociceptors may detect ‘danger’ messages in response to noxious or painful stimuli, but this isn’t always the case. Nociceptors can activate even in the absence of a painful stimulus. Take, for example, this story of a 29-year-old construction worker. A nail penetrated his boot and he felt excruciating and unbearable pain immediately. Doctors had to give him strong pain medication to help take the edge off. Turns out, the nail never pierced his skin, it went right between the toes.[1] No direct injury to tissues but the pain he experienced was very real.
Ultimately, the interpretation of pain is determined by your brain that weighs the world for you. Not all danger messages are harmful or hurtful. How you interpret these messages is based on a hodgepodge of factors, including:
- Past experiences
- Environment
- Beliefs
- Thoughts
- Values
- Understanding and knowledge
- Safety
- Current situation
- Expectations
- Perspective
- What healthcare providers told you
- Social taboos
- Religious views

I say ‘you interpret…’ because, well, your brain is you!
With persistent pain, the tissues have long since healed but the message in your brain stays the same: that you’re in danger. When you have ongoing pain, the signals to your body from your brain have strengthened, making the signal sharper. Pain always wants to know what’s going on, so it’s only natural for danger sensors to sprout and recruit other neighboring tissues to join in on the conversation.
This means your pain might seem like it’s playing tricks on you. First it’s here, then it’s there, jumping around all over the place. Pain and muscle tension respond to a ‘perceived’ threat but that doesn’t necessarily mean being directly in harm’s way.
So, what can you do about it? My advice here is to get a new mantra: ‘I’m sore but I’m safe.’ (Big thanks to David Butler for the inspiration.)
If you’re experiencing persistent pain, know that you’re not alone and that there’s hope. The more you understand why you hurt, the less you will hurt.
Although
uncomfortable and at times life-altering, pain doesn’t have to be scary.
Working with a professional who listens to your story and can help you make
sense of your pain experience is a key ingredient for your recovery. So if
you’re ready to tame your pelvic pain, let’s chat.
[1] Derbyshire, SWG. (2011). Can Neuroimaging Explain Pain? Psychiatr Clin N Am, 34, 595-604.