Celiac disease affects 1 in 100 people worldwide (1). It can develop at any age and can lead to serious health problems if left untreated. Currently, the only treatment is a strict, gluten-free diet, therefore early diagnosis is crucial for reducing long term complications.
What Causes Celiac Disease?
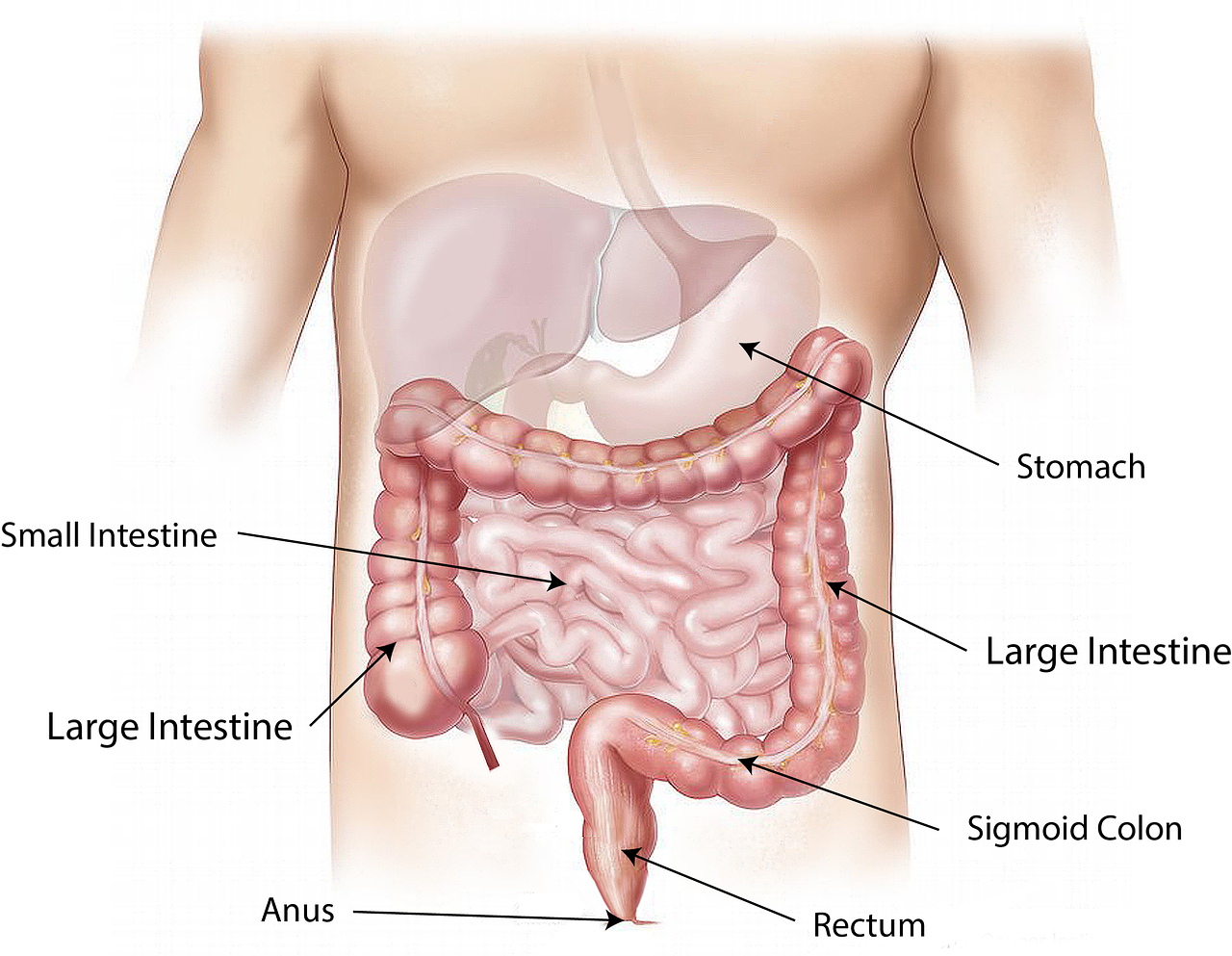
A long-term autoimmune disorder, celiac disease affects the small intestine and is characterized by mucosal inflammation, villous atrophy, and crypt hyperplasia (2). Some of the manifested symptoms are diarrhea, loss of appetite, and abdominal distension. Individuals may also develop iron deficiency anemia due to malabsorption of nutrients in the intestine. However, it is also possible for someone with celiac disease not to experience any symptoms at all (2).
Celiac disease occurs upon exposure to dietary gluten, or the protein gliadin, that can be found in the endosperm of some cereal grains such as wheat, barley, and rye. These proteins are rich in proline and glutamine, and are resistant to the enzymatic digestion of proteases and peptidases of the gut (2).
Genetically, celiac disease has been linked to a protein produced by the body called HLA-DQ. The HLA-DQ protein is part of the MHC class II system that triggers the normal immune response (3). Each individual has one of two types of the protein, encoded by the HLA-DQA1 and HLA-DQB1 genes. One of two specific isoforms of HLA-DQ, the DQ2 or DQ8, is present in 95% of people diagnosed with celiac disease. These two types of HLA-DQ are inherited, and the expression of the genes HLA-DQ2 or HLA-DQ8 results in the synthesis of specific receptors that bind tightly to gliadin. These receptors will initiate the autoimmune response when gluten is ingested, as they have more affinity to gliadin than regular receptors (3).
It has been studied, however, that there are often other factors that can cause celiac disease. A small number of the patients do not have these HLA-DQ alleles, and strikingly, a vast number of people without this disorder have one of these two alleles. Due to these cases, research is still actively focusing on causes of celiac disease as its complexity is not yet fully understood.
Present and Future of the Disease
Early diagnosis of celiac disease is difficult, as less than 50% of adult patients present the classic gastrointestinal symptoms. Surprisingly, current knowledge of the gluten-free diet as the only available and accepted treatment dates back to the 1940s (4).
Studies are aiming to explain the main molecular mechanisms and the protein-protein interaction networks involved in celiac disease in order to provide laboratories with the tools to develop a sophisticated drug. Understanding these networks can contribute to the discovery of the pathogenesis biomarkers. The main goal is to develop therapies that can improve the quality of life for patients and also help them to avoid long-term health complications such as osteoporosis, infertility, pancreatic insufficiency, and neurological manifestations. Even more seriously, celiac disease has been associated with type 1 diabetes mellitus, psoriasis, hepatitis, and other chronic conditions (5).
It is possible that celiac disease is linked to many other severe diseases in ways that are currently unknown. Further research is the only way to fully understand the diverse metabolic pathways that are relevant to this condition, which can lead to better treatments and early disease prevention.
Sources
- https://celiac.org/about-celiac-disease/what-is-celiac-disease/
- Zamanian Azodi M, et al. Protein-protein interaction network of celiac disease. Gastroenterol Hepatol Bed Bench. 2016 Autumn; 9(4): 268–277.
- Megiorni F, Pizzuti A. HLA-DQA1 and HLA-DQB1 in Celiac disease predisposition: practical implications of the HLA molecular typing. J Biomed Sci. 2012; 19(1): 88.
Published online 2012 Oct 11. doi: [10.1186/1423-0127-19-88]
- Castillo N, et al. The present and the future in the diagnosis and management of celiac disease. Gastroenterol Rep (Oxf). 2015 Feb; 3(1): 3–11. Published online 2014 Oct 17. doi: [10.1093/gastro/gou065]
- Nahid Safari-Alighiarloo, et al. Protein-protein interaction networks (PPI) and complex diseases. Gastroenterol Hepatol Bed Bench. 2014 Winter; 7(1): 17–31.