Brain Injury in Service and its Relationship to Mental Health
Concussion Legacy Foundation
Author: Samantha Bureau, PhD
In September, we come together to raise awareness about concussions so that more individuals and families know what to do in the event they or their loved one sustains one.
A concussion is a type of traumatic brain injury, or TBI, caused by a bump, blow, or jolt to the head or by a hit to the body that causes the head and brain to move rapidly back and forth. While concussions are usually not life-threatening, we still need to treat them seriously as the effects of a concussion can change a life.
This Concussion Awareness Month, we especially want to raise awareness that concussions do not exclusively happen in sport.
While we often see and hear stories about former contact and collision sport athletes struggling with the impacts of single and repeated brain injuries, we know that brain injury impacts a far broader demographic, including kids on the playground, accident survivors, and those with higher risk occupations, such as our service members and first responders. Some ways brain injury may occur within this community include airborne training, breaching, exposure to blast, combat training, firing artillery, sports participation, falls and accidents, and motor vehicle collisions.
According to the DOD Traumatic Brain Injury Center of Excellence, more than 485,000 service-members sustained a traumatic brain injury since 2000.[1]
We also know that brain injuries are largely under-reported, so there are likely many more service-members who have sustained a brain injury in service, and many more who sustained a brain injury outside of service in their day to day lives. We also know that our first responders are at risk of brain injury. A recent study on first responders showed an alarming 74% of police officers studied reported a history of at least one brain injury, with 30% reporting at least one injury sustained on the job.[2]
This study also noted that many of these injuries went unreported and untreated.

Without the help of a medical provider and proper treatment following a brain injury, the likelihood of prolonged symptoms and difficulties increases. This is why recognizing and reporting brain injuries is of the utmost importance.
In the event you or your loved one sustains a concussion, here are some signs and symptoms to be aware of:
Concussion Signs Include:
- Problems with balance
- Glazed look in the eyes
- Amnesia
- Delayed response to questions
- Forgetting an instruction, confusion about an assignment or position, or confusion of the game, score, or opponent
- Inappropriate crying
- Inappropriate laughter
- Vomiting
- Loss of consciousness
Common Concussion Symptoms:
-
Somatic (Physical) Symptoms
- Headache
- Light-headedness
- Dizziness
- Nausea
- Sensitivity to light
- Sensitivity to noise
-
Cognitive Symptoms
- Difficulties with attention
- Memory problems
- Loss of focus
- Difficulty multitasking
- Difficulty completing mental tasks
-
Sleep Symptoms
- Sleeping more than usual
- Sleeping less than usual
- Having trouble falling asleep
-
Emotional Symptoms
- Anxiety
- Depression
- Panic attacks
As we continue to learn more about how concussion impacts this community, one area of research that has gained attention more recently is on the relationship between brain injuries and mental health outcomes.
A 2019 systematic review and meta-analysis from researchers at Harvard University researchers has shown that a single traumatic brain injury can double your risk of suicide.[3]
And this is not the only study that has linked negative mental health outcomes to brain injury. A 2022 study from the Children’s Hospital of Eastern Ontario (CHEO) demonstrated that children diagnosed with a concussion were 40% more likely to develop a new mental health disorder following their injury than children diagnosed with an orthopedic injury.[4]
But does this also apply to our service members and first responders?
The answer is yes.
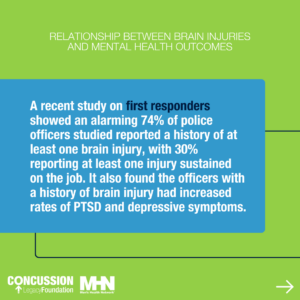
A 2023 study reviewed the records of more than 860,000 US military service members and demonstrated that soldiers with military related traumatic brain injury had significantly higher rates of new-onset mental health conditions than those without a TBI. Those individuals were also at increased risk for suicide.[5] Additionally, the study that showed 74% of police officers reporting a history of brain injury also found the officers with a history of brain injury had increased rates of PTSD and depressive symptoms than those who did not report a history of brain injury.2
If you are reading this and are struggling with the impacts of brain injury, we are here for you.

Whether your injury was recent or years ago, if you are still experiencing symptoms and don’t know where to turn, the Concussion Legacy Foundation can help.
Our CLF HelpLine and Peer Support programs offer opportunities for you to get the help you need from a trusted team.
Whether you need help finding medical providers in your area, or you are just looking for someone to talk to who understands your situation, we encourage you to reach out to us at CLFHelpLine.org.
About Samantha Bureau, PhD
Dr. Samantha Bureau is a Canadian neuroscientist specializing in neurodegenerative diseases, known predominantly for her work investigating brain injuries and chronic traumatic encephalopathy. During her doctoral training, she specialized in the cellular and molecular medicine of Parkinson’s and Alzheimer’s, investigating therapeutic targets to alter disease progression. Dr. Bureau has had the privilege of educating military personnel at NATO exercises, and engaging the highest-ranking officials of the Canadian Armed Forces, the Brain Injury in Sport Working Group in the UK, and the Federal-Provincial-Territorial Working Group on Sport in Canada. Notably, her work has inspired change around the world, influencing the NIH, NHS, PFA, AFL, and the Australian Senate Committee, among others, to update their views on CTE causation.
Prior to joining the Concussion Legacy Foundation, Dr. Bureau worked at top-tier academic research institutions including the Boston University CTE Center and the University of Ottawa Brain and Mind Research Institute. She currently serves as the Director of International Programs at CLF where she oversees the foundation’s patient services programs, international operations, and ongoing global research initiatives and collaborations.
Dr. Bureau is a former dual-sport NCAA athlete in ice hockey and outdoor track and field. She received her PhD in Neuroscience from Carleton University and her MBAs from Cornell University and Queen’s University.
References:
[1] DOD Traumatic Brain Injury Center of Excellence. https://www.health.mil/Military-Health-Topics/Centers-of-Excellence/Traumatic-Brain-Injury-Center-of-Excellence/DOD-TBI-Worldwide-Numbers
[2] Caccese JB, Smith CR, Edwards NA, et al. Silent Struggles: Traumatic Brain Injuries and Mental Health in Law Enforcement. J Head Trauma Rehabil. Published online August 5, 2024. doi:10.1097/HTR.0000000000000986
[3] Fralick M, Sy E, Hassan A, Burke MJ, Mostofsky E, Karsies T. Association of Concussion With the Risk of Suicide: A Systematic Review and Meta-analysis. JAMA Neurol. 2019;76(2):144-151. doi:10.1001/jamaneurol.2018.3487
[4] Ledoux AA, Webster RJ, Clarke AE, et al. Risk of Mental Health Problems in Children and Youths Following Concussion. JAMA Netw Open. 2022;5(3):e221235. Published 2022 Mar 1. doi:10.1001/jamanetworkopen.2022.1235
[5] Brenner LA, Forster JE, Gradus JL, et al. Associations of Military-Related Traumatic Brain Injury With New-Onset Mental Health Conditions and Suicide Risk. JAMA Netw Open. 2023;6(7):e2326296. Published 2023 Jul 3. doi:10.1001/jamanetworkopen.2023.26296